Chronic Kidney Disease (CKD) prevention
Adopting below measures can surely prevent the progression of chronic kidney disease and prolong the renal function and thus avoid early need for renal replacement therapy.
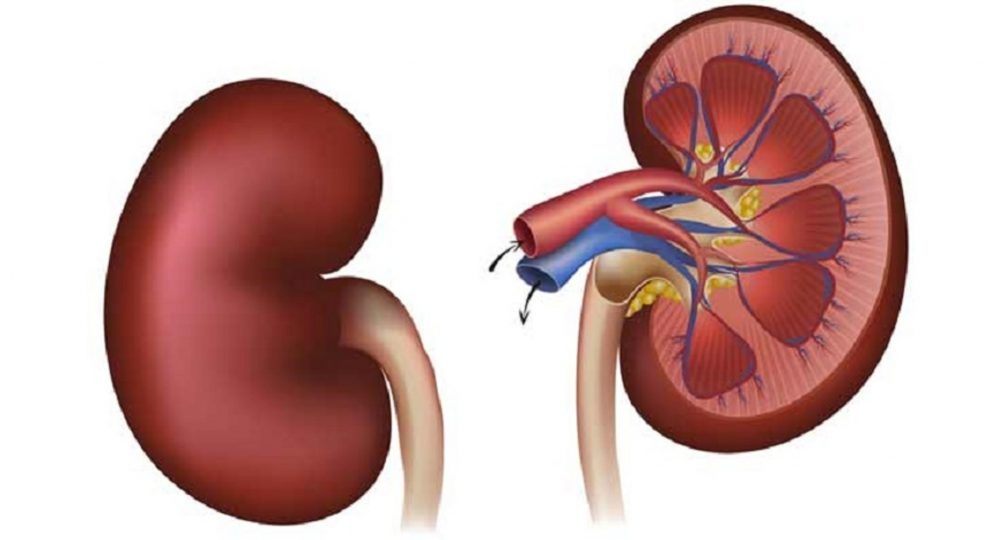
Kidneys are crucial organs and life is at risk when kidneys don’t work properly anymore. It not only balances the volume of water and eliminate the waste products from the body, but also produce hormones that regulate some important body functions like regulating blood pressure, making of red blood cells in blood and strengthening bones.
Chronic kidney disease (CKD) is the presence of kidney damage, or a decreased level of kidney function for a period of 3 months or more. It usually affects both kidneys. It is common, harmful but often treatable in early stages. Prevalence of CKD is around 8 -12 % of the adult population with probable annual Increase in incidence of 10-12%. A person once diagnosed with CKD, need to take care of their kidney function for the rest of their lives. CKD can trigger other health issues (cardiovascular diseases) leading to premature death or disability. If not detected early enough, it may progress to kidney failure which then requires renal replacement therapy (RRT) in form of dialysis or a kidney transplant to survive.
Who is at risk?
Although there are many causes of CKD, the two most predominant causes are diabetes and high blood pressure. The other risks for developing kidney disease are positive family history, obesity, prolonged pain killer or drug abuse, existing severe cardiovascular disease and aging.
Screening for CKD
Early kidney disease often has no symptoms. Early detection is therefore very important to prevent the progression of the disease. Screening of the CKD is needed in patients who are having risk factors. Standard screening tests are blood test (Kidney function test) to calculate e-GFR and measurement of urinary protein or microalbumin.
Stages of CKD
Based on e-GFR, the chronic kidney disease is staged starting from stage I minimal loss of renal function (<10%) GFR >90 ml/min/1.73 m2, stage II GFR 60-90 ml/min/1.73 m2, stage III GFR 30-60 ml/min1.73 m2, Stage IV GFR 15-30 ml/min/ 1.73 m2 and stage V severe loss of renal function or end stage renal disease (renal failure) GFR <15 ml/min/ 1.73 m2.
Why prevention is important?
Although it’s scary for a person to be diagnosed with chronic kidney disease but even if someone is diagnosed in early-stage CKD (stage 1-3), there are many steps a person can take to preserve the existing renal function and delay the further loss of renal function. One need to work closely with his doctor and there are good chances that he can still enjoy a healthy life even with existing kidney disease.
Steps to prolong kidney function
Once a person develops CKD, there are actions an individual can take to prolong kidney function. This includes treatment of the underlying conditions i.e. control of diabetes, hypertension and proteinuria, avoidance of nephrotoxic drugs, dietary and lifestyle changes like stopping smoking & regular exercise.
Control of blood pressure
Aggressive blood pressure control can help in delaying the decline in renal function in patients with CKD. The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (KDOQI) suggest a target blood pressure of less than 130/80 mm Hg. Systolic blood pressure (SBP) control is considered more important than diastolic blood pressure control.
Diabetes and prolonging kidney function
In diabetic patient, the hemoglobin A1c (test to check optimum sugar control) should be kept below 6.5 percent and kidney function tests should be performed at least once in 6 months. In CKD, a hemoglobin A1c (HbA1c) level higher than 9% is associated with worse clinical outcomes.
Treatment of Proteinuria
Drugs like ACEIs or ARBs are routinely prescribed in diabetic kidney disease with or without proteinuria. However, in nondiabetic kidney disease, these agents are also effective in retarding the progression of disease among patients with proteinuria of more than 500 mg/day.
Calcium & Vitamin D supplementation
Routine use of calcium and vit D is recommended in all CKD patients not only for maintaining good bone health but also to delay progression of the disease. Daily vitamin D supplementation decreases albuminuria in patients with stage 3-4 CKD who had low vitamin D levels and high parathyroid hormone (PTH) levels.
Avoid Nephrotoxins
A great number of individuals with CKD may be unaware of their disease and thus may be at risk for further kidney injury through use of NSAIDs. They should inform about their renal function status before start of any antibiotics for adequate selection and titration of doses to avoid nephrotoxicity.
Management of metabolic acidosis
Correction of acidosis with sodium bicarbonate is associated with significantly slower progression of CKD. Achieving target serum bicarbonate levels (24-28 mmol/L) required an average of about 6 g/day of sodium bicarbonate (two to four tablets) taken twice daily.
Management of cardiovascular risks
Improving Global Outcomes (KDIGO) workgroup recommend that all adults with newly diagnosed CKD should undergo lipid profile testing. Adults aged 50 years or older with CKD and an e-GFR of 60 mL/min/1.73 m2 or higher should be treated with a statin.
Dietary modification
Plant-based diets delays progression to ESRD and dialysis and potentially improves survival. Increasing the alkali-inducing fruits and green leafy vegetables in the diet may help to reduce kidney injury.
Protein restriction
The Modification of Diet in Renal Disease (MDRD) Study suggested that a low-protein diet slows down the GFR decline and reduces proteinuria.However, if a patient is started on protein restriction, closely monitoring of the patient’s nutritional status is very important. Protein restriction is not recommended in paediatric patients with CKD. About 56 grams of protein each day will easily provide the average protein needs for a man who weighs 60 kg. One should avoid red meat (beef, bison, lamb, pork, venison & organ meats like liver etc.)
Salt restriction
Reduction in salt intake slows the progression of diabetic CKD by lowering blood pressure. In general, a healthy amount of sodium is 2,300mg (1 teaspoon of salt) or less per day. Avoid taking salt substitutes as these are made with potassium and could raise the potassium to a dangerous level. Encourage preparing meals at home to control the amount of salt in the food. Drink water instead of sports drinks or soda.
Other dietary restrictions
The following other dietary restrictions are also indicated:
Phosphate restriction (starting early in CKD): Avoid meat, sea food, nuts and milk or milk product more than 500 mg/day.
Potassium restriction (Avoid potassium rich foods like banana, avocado, citrus fruits, potato, beans, spinach and fish).
Water restriction (specially in higher stage) as needed to avoid volume overload.
Life style changes
Smoking should be strictly avoided as this decreases the risk for future onset of kidney failure.Patients with CKD should also undertake regular exercise, as compatible with cardiovascular health, ideally for at least 30 minutes 5 times per week.
Adopting above measures can surely prevent the progression of chronic kidney disease and prolong the renal function and thus avoid early need for renal replacement therapy.

